Deformity Correction
About Deformity Correction
Deformity correction– Bony and joint Deformity can occurs because of many reasons. Etiology in both children and adult are different. In children it occurs because of congenital, trauma, infection and developmental reason. In adult it can occur because of trauma and infection and also as sequels of pediatric problem. leg deformities affect muscle, bone and joint. With the popularization of external fixater and invention of concept of distraction osteogenesis by the Prof. GavriilIlizarov in Russia in 1950’s deformity correction, malunion and nonunion of fracture management became much easier. In 1990 onward Dr. Drohr Paley give many concept of deformity correction that changed whole concept of deformity correction. Deformity correction can be done by many methods which include open bony osteotomy, Ilizarrov, Rail fixater system, growth modulation. Tendon lengthening, tendon transfer etc.
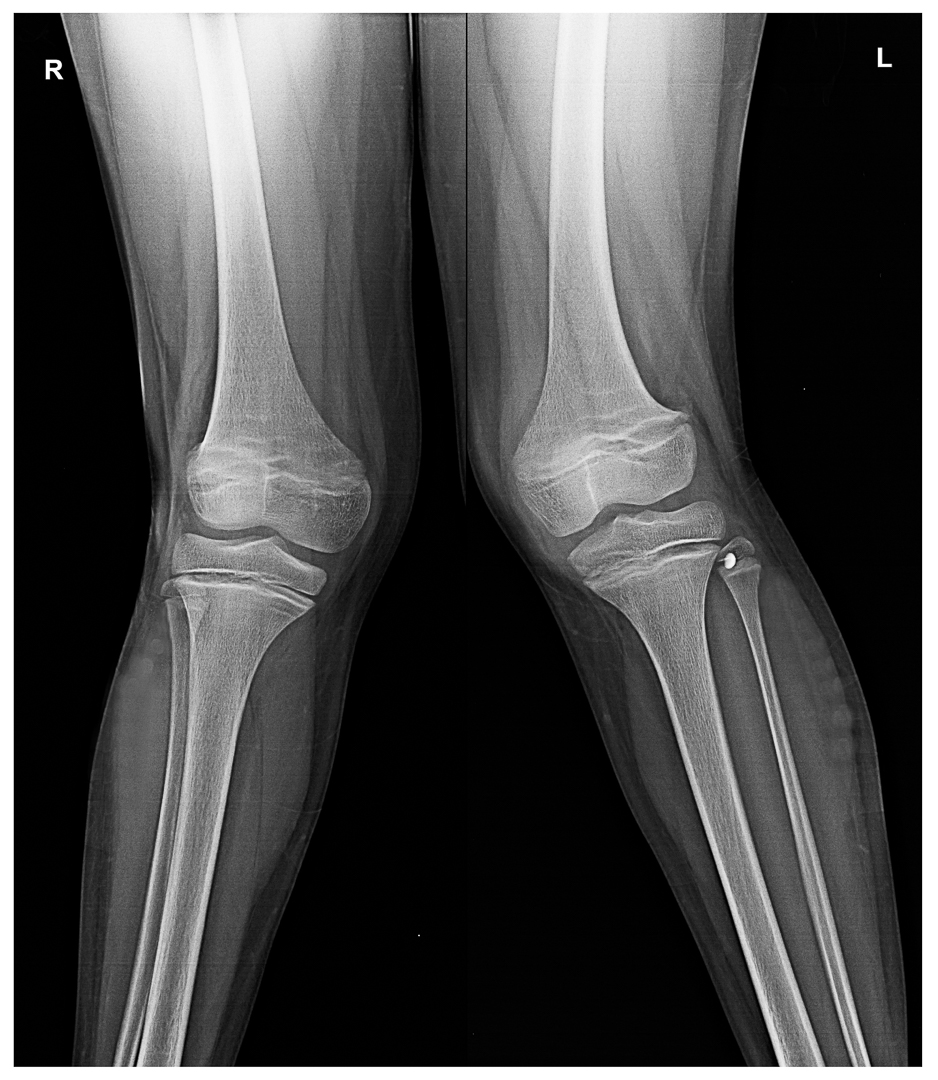
Genu valgus (Knock Knee treatment) – it is a condition in which both knee touches together and foot is wide apart in standing. This condition is commonly occur because of Vit D deficiency in children. Other causes are physial injury, infection and bony dysplasia etc. It is physiological in very young children of 3 to 6 year age. But it is mild. Distal femur is the most common location of pathological genu valgus. Physiological genu valgus resolve by the age of 7 year. Inter malleolus distance should not be more than 8cm at the age of 7 year.
Investigation:
Standing X-Ray AP View of both lower limb with patella facing forward is required for measurement of diagnosis, causes and measuring angle of deformity
Treatment:
< 6 year age with < 15 degree of genu valgus— Observation, Vit D, Calcium supplements, usually resolve with growth
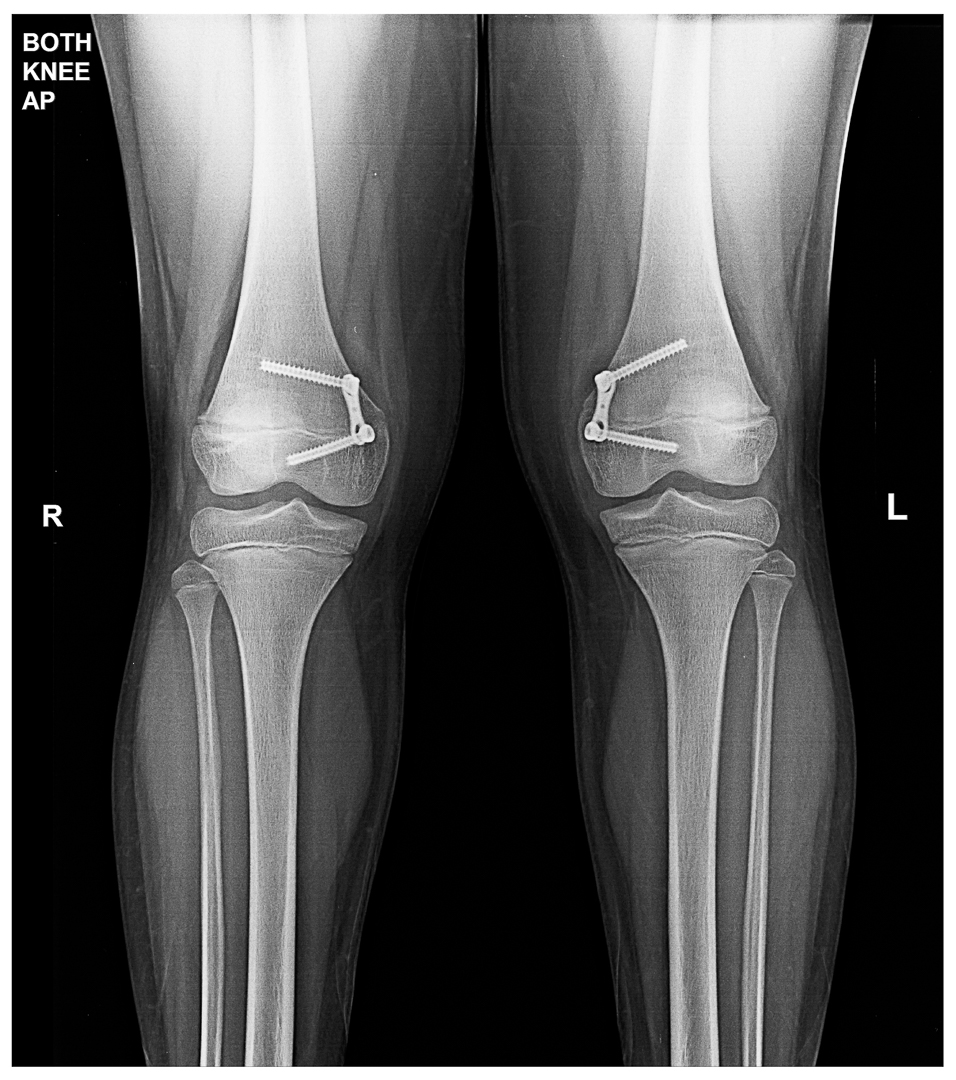
< 12 year age in female < 13 year in male with sufficient remaining growth :Growth modulation / hemi-physiodesis of distal femur physis / tibia proximal tibial physis (rare)
Corrective osteotomy in matured and adults.
Genu varus (bow leg, tibia vara)– it is a bowing of tibia. It is physiological below the age of two year. It will be symmetrical and painless bowing. This problem resolve spontaneously before the age of 3 year without any treatment as a results of normal growth. Parenteral counselling and assurance is required.
Pathological genu varus: in young children it occur because of vitamin D deficiency. Due to Vit D deficiency, bone are very soft, physical plate became widen so with weight bearing bone bends. In vit D deficiency tibial bowing is the commonest deformity. Vit D deficiency can occurs because of Nutritional deficiency, kidney disease, hypophosphatemia.
Other causes-
Blount Disease- it is the growth disturbance of proximal medial tibia that can present any time from infancy to adolescent. Mostly related with morbid obesity. In very early age < 5 year deformity can be corrected by growth modulation but afterward they need very complicated surgery.
Skeletal dysplasia: Achondroplasia, multiple epiphyseal dysplasia, metaphyseal dysplasia are the common causes. Other associated feature like short stature, multiple bone & joint involvement, specific spinal deformity will be present in these cases.
In adult: continuation of child hood problem, familial tibial bowing, trauma are the common causes of tibial bowing and varus knee deformity. With severe knee varus deformity, weight thrust is more on medial tibial condyle so patient develop osteoarthritis of knee joint in long term.
Investigation:
Clinical examination is sufficient for making diagnosis but to see the etiology we need radiological evaluation like weight bearing full length X-ray of both lower limb in standing. X-ray give sufficient information of etiology and severity. In some patient we may need VitD assessment.
Treatment :
Except physiological variety in very young children <2 year age, all other variety need surgical correction. Bracing has no role in treatment of genu varum. Growth modulation (hemiphysiodesis) can be done in children with sufficient remaining growth of physis. Hemiphysiodesis can be done by the plate, screw, staple application at convex side of growth plate. For pediatric orthopedic in Prayagraj, consult with specialists for appropriate diagnosis and treatment plans
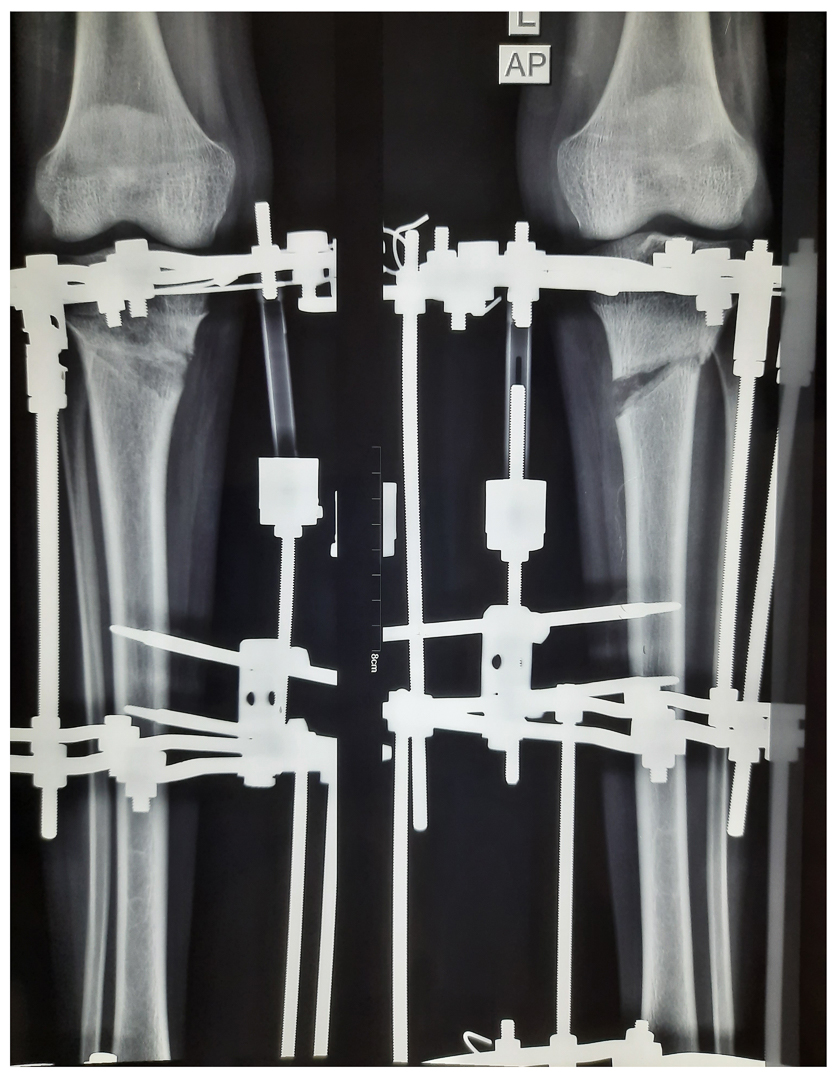
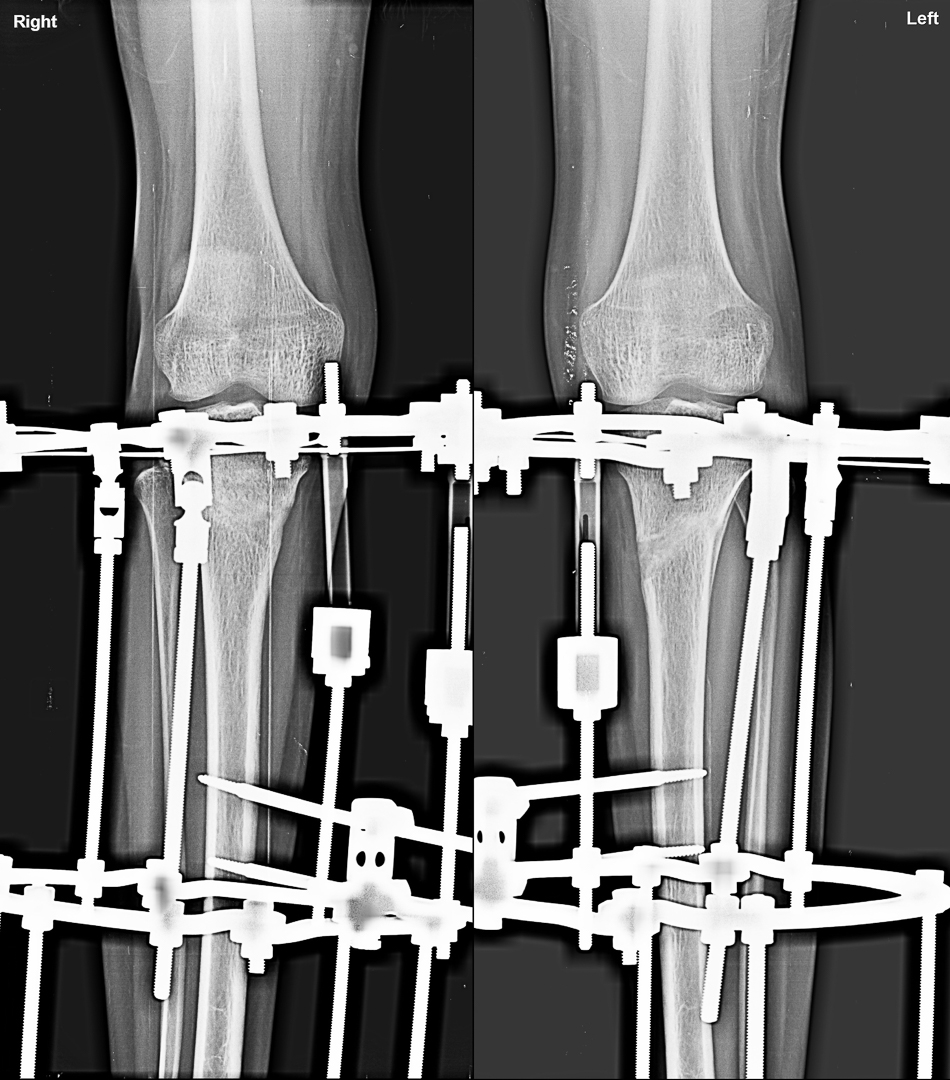
Osteotomies is required in patient where growth of bone stopped further or very sever deformity where growth modulation will unlikely to correct that much deformity. Osteotomy can fixed by plate or external fixater system
Gradual correction by corticotomy and bone transport by LRS System/ ilizarov.
Spina Bifida-— it is a type of a neural birth defect. In this problem a portion of neural tube does not close or develop properly, causing defects in the spinal cords and in the bone of spine. Spina bifida can present from mild to sever abnormality.
Types:
Spina bifida occulta: it is the mildest and most common type. It results in small gap in one or more bone.
Meningocoel: a sac fluids comes through an opening in child back. But spinal cord is not in the sac. there is no or little neural damage.
Myelomeningocele: it is severe form of spina bifida. In this condition, a sac of fluids comes through an opening in baby’s back. Part of spinal cord and nerve are present in the sac. This type of spina bifida causes moderate to severe disability depending upon level of lesion in spine.
Diagnosis: spina bifida occurs because of neural tube defects. Except spina bifida occulta, It can diagnosed in utero as well after delivery.
During pregnancy ultrasound helps a lot in identifying the neural tube defects. Alfa-feto protein level also helps in identifying neural tube defects.
After delivery: diagnosis& severity of spina bifida is defined by xray, mri of spine.
Prevention: folic acid supplements during pregnancy prevent significant percentage of spina bifida from developing in fetus. It is better to start folic acid before planning for pregnancy. Diabetes and obesity should be taken under control during pregnancy.
Treatment :
Spina bifida occulta diagnosed very late because it is not identifiable so easily. It does not create much problem except backache in late age.
Meningocoele also don’t create problem except sac containing fluid and meninges that has to operate in early phase of life.
Meningo-myelocoel need consideration. Because it can cause severe disability like weakness, paresis in both lower limb, bladder bowel involvement etc. defect in the spine should be closed after birth by the pediatric / neuro surgeon. Initially limb will be flail but depending upon level of defect, they remain flail or become spastic. So proper positioning, exercise and bracing is must to prevent deformity. Disability can vary from trivial problem to severe disability. Deformity should be corrected for proper brace fitting and mobilization.
For More Information: Pediatric Orthopedic Treatment FAQs
Genu Valgus managed by Growth Modulation:
Genu Valgus corrected by Bone Osteotomy
Genu Varus corrected by Osteotomy and gradual correction with Ilizarov
Meningomyelocoel with difficult deformity rt knee and ankle managed by osteotomy
Post Osteomyelitis Distal Femur Deformity
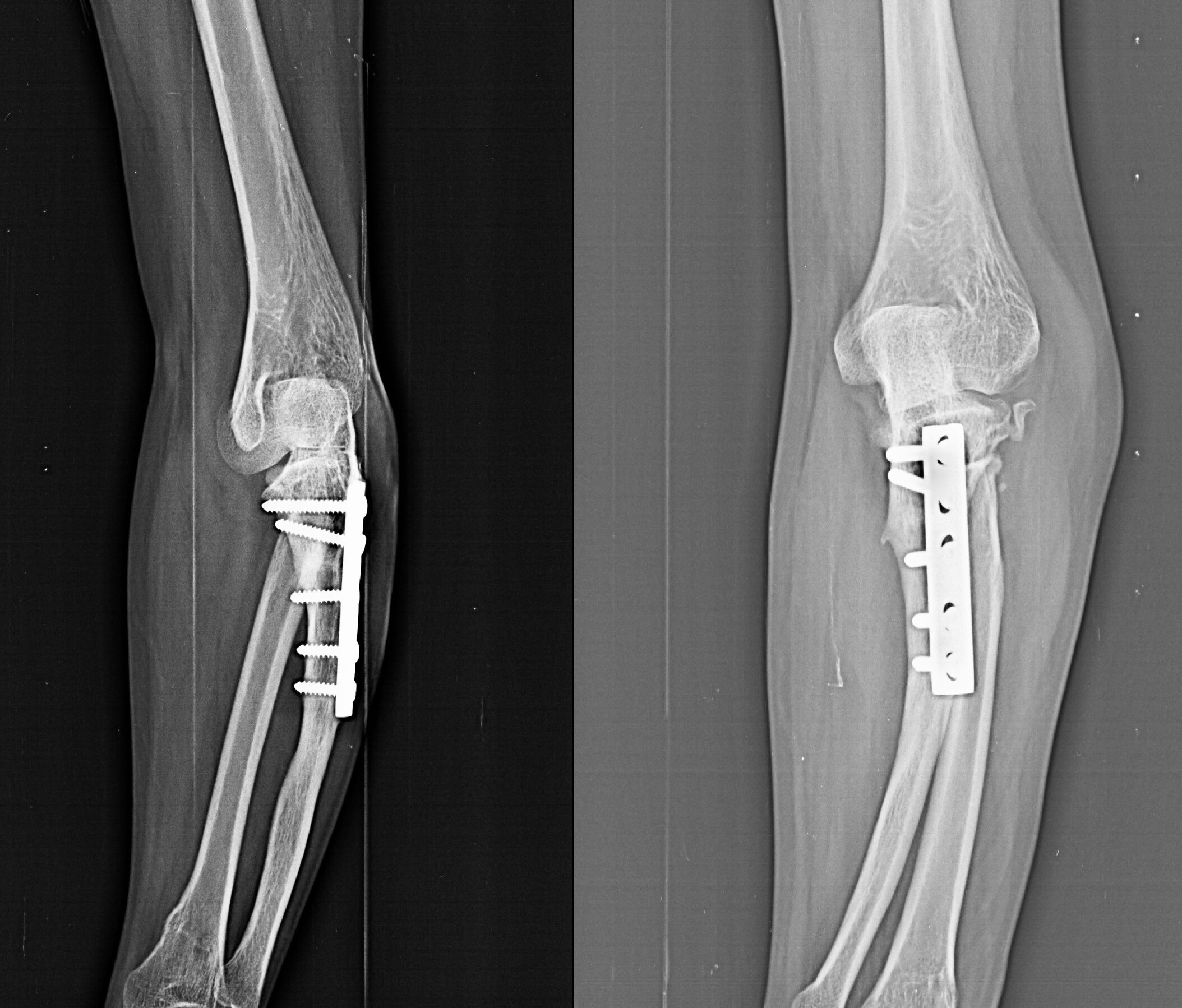
Post-traumatic Elbow Deformity
Proximal Tibia Deformity and Shortening
Reviewed and Submitted by Dr. Jitendra Kumar Jain
Last updated on July 11, 2020
Dr.Jitendra Jain, MD and DNB (Orthopedics), president at Trishla Foundation, an NGO for treatment of cerebral palsy, and a Consultant Pediatric Orthopedic Surgeon & Cerebral Palsy Specialist at Trishla Orthopedic Clinic & Rehab Center.
Dr. J. K. Jain is a member of the general council at Dr. SMN university of rehabilitation, Lucknow, a member of the advisory board chief commissioner for PWD, Govt. of India (New Delhi), a member of the state disability research committee (U.P.), and a member of the committee of RCI, New Delhi. He has been awarded many awards, including the Dr.Bhagawan das memorial award, the spirit of humanity award, and the state govt. award for his services towards PWD, etc. Times of India has posted his work many times and mentioned him as one of the best doctors in the field of Pediatric Orthopedics. He helped many children recovering from cerebral palsy, just like comedian jay Chanikara, who is now able to stand and walk without any support, Abena, a Ghana girl with cerebral palsy, and many more. He also organized the National Wheelchair cricket tournament and created World’s first cerebral palsy village foundation in Prayagraj. He successfully treated 10,000+ children with various kinds of orthopedic disability, conducted 160+ free assessment camps, and produced a documentary film on cerebral palsy.
Walk in Appointments Available Daily
You can make an appointment online for video tale-consultation by fixing up an appointment at this website or you can visit the clinic to make an appointment in person and show to doctor with the care of social distancing at the given time.
Contact us
Call Us
0532-2468989
+ 91 9415014994
+ 91 8577873545
+ 91 9455001645
Email Us
totrishlaortho@gmail.com
Our Location
Dr. Jitendra Kumar Jain
Trishla Orthopedic Clinic & Rehab center, 182C / 350A, Tagore Town, Prayagraj (Allahabad) U.P-211002, India