Legg-Calve-Perthes Disease Treatment
Introduction of Perthes Disease:
Perthes disease is also known as Legg-calve-Perthes disease.
- It is a rare childhood condition that affects the hip joint.
- It may affect one or both hips.
- The usual age of presentation is 4-12 years old.
- It developed in stages.
- In this disease blood supply to the femur head and neck is temporarily hampered.
- Because of interrupted blood supply, bone cell die. This process is known as avascular necrosis.
- After the avascular necrosis, bone of femoral head became too soft. Rounded shape of the femoral head is disturbed due to stresses of weight bearing, joint movement, muscle spasm.
- Blood supply will be restored with passage of time.
- Once blood supply restored, femoral head start taking shape.
- In certain cases, rounded shape don’t came again.
disease is also known as Legg-calve-Perthes disease. It is a childhood condition that affects the hip joint. In this disease blood supply to the femur head and neck is hampered. Because of interrupted blood supply, the rounded shape of the femoral head is disturbed. It may affect one or both hips. The usual age of presentation is 4-12 years old. It developed in stages.
Causes of Perthes Disease:
Disturbance in blood supply is the common cause. Causes for vascular insult is unknown Genetic & environmental factor have been implicated
Two Aetio-pathogenesis:
- Formation of blood clots in blood vessels of femoral blood due to
Blood clotting disorder
Blood cell morphology like sickle cell anaemia,
- Decrease in blood supply to the femoral head.
Stages in Perthes Disease:
- Stage 1: Sclerosis/ Necrosis- Infarction produces smaller & sclerotic epiphysis
- Stage II: Fragmentation- Femoral head appears fragmented
- Stage III: Healing Stage (Reossification) – New bone formation
- Stage IV: Residual (Healed) Stage- Femoral head remodel till skeletal maturity
Symptoms of Perthes Disease:
- Earliest sign of Perthes disease is the painless limping that means child is not able walk & run properly.
- Other symptoms start once it progress are:
- Pain in hip, groin & knee
- Shortening of limb
- Restriction of hip movement like hip flexion, abduction, rotation
- Not able to squat or sit in cross leg.
Tests for Perthes Disease:
Initially doctor will take detail history, how it happen, duration & symptoms. Then doctor will examine the child in detail.
You need to have check up with paediatric Orthopaedic surgeon
Physical assessment Test:
Doctor will see the range of movement at hip joint, restriction of movement, shortening.
In Perthes most common restriction is abduction (taking leg to outside from hip joint) & internal rotation (twisting of leg inside)
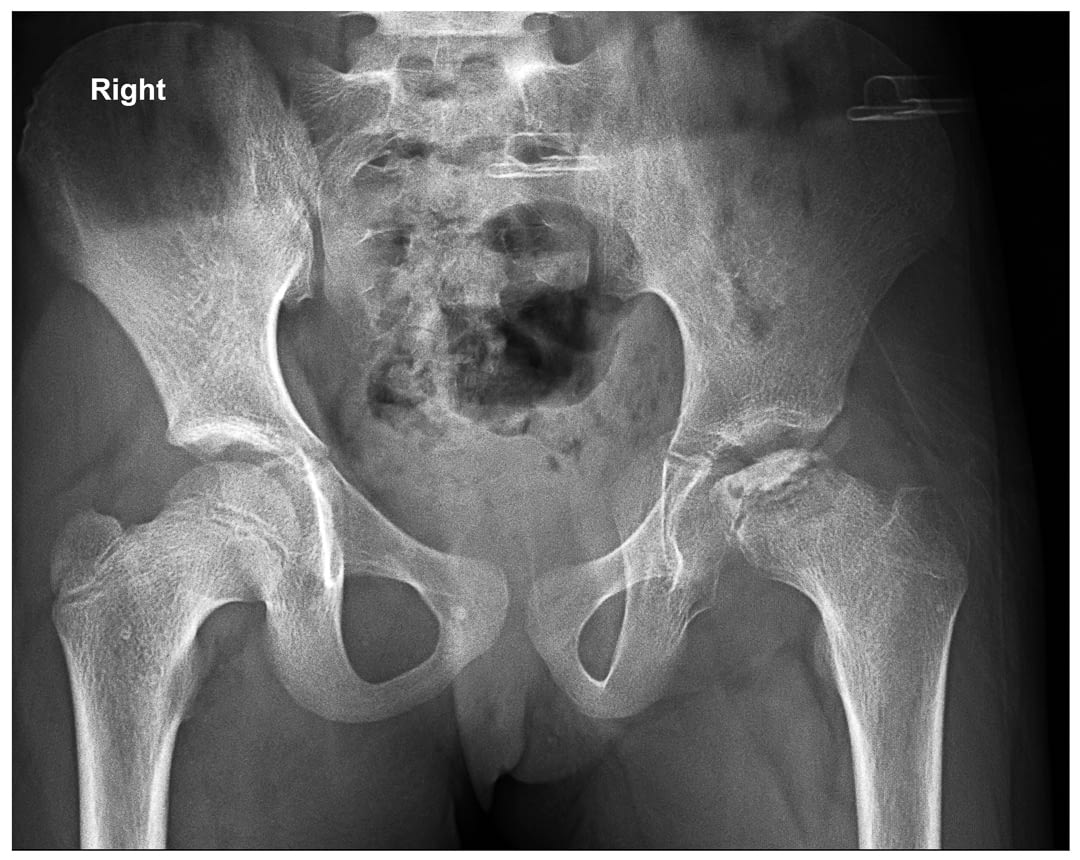
X-ray:
X-ray of both Hip joint will be taken in two different direction (anteroposterior & lateral view). With the x-ray doctor will see the bony abnormality of proximal femur. Repeated X-ray evaluation is required to see the progress of child in total period of treatment.
MRI:
MRI are needed to rule out other causes and see then exact damage in femoral head.
How Perthes Disease diagnosed in a child?
- Perthes disease is being diagnosed by the specific history of painless limping in start and then painful restriction of hip movement, radiating pain to knee, inability to squatte or sit cross legged.
- Child need to be assessed in detail by pediatric orthopedic surgeon in india in detail.
- For final confirmation of diagnosis doctor may need x-ray to see the clear image of damage in hip joint and impact of avascular necrosis.
- MRI will show ischaemic insult in the femoral head. Some time it became very difficult to differentiate from other cause like tuberculosis etc.
Avaliable Treatment for Perthes Disease
- Most of the problem in Perthes is self-limiting but we need to protect the shape of femoral head & preserve hip joint movement.
- If left untreated then femoral head will deform & will not fit into acetabulum cavity.
- This unmatch surface of joint will cause early arthritis in adulthood.
Treatment is depend upon many factor:
Non-Surgical Treatment of Perthes Disease:
- Age of Child:
- Lesser the age of child (<6 year), better potential for good recovery
- More the age (>9 year) more chance of surgical intervention & guarded outcome.
- Degree of femoral head involvement: More the area of femoral head is involve, poorer will be the prognosis.
- Stage of disease at time of treatment: Perthes disease develop in stages so treatment modality will be decided at which stage treatment was planned.
Treatment: Containment:
Containment means putting the femoral head (weight bearing surface) inside acetabular cavity. Containment is very important for normal growth of femoral head. It can be done through plaster/ brace/ bony surgery
Non-Surgical Treatment of Perthes Disease:
Observation: In early age onset 2-6 year age, only observation and repeated x-ray is required. Most of time they heal very well without any long term impact.
Medicine: Analgesic are being used to treat pain & spasm. But long term use can cause gastritis so without consultation with doctor, child should not be given analgesics.
Avoidance of sport: Femoral head bone are very soft in Perthes so child should be advised to refrain from running, jogging & sport activity for time being.
Exercise: Restriction of hip movement is very common.
So to regain joint movement child need to do hip abduction & rotation exercise. But before start of exercise child should be examined by paediatric orthopaedic surgeon / physical therapist. Femur head may touch the acetabular margin on abduction & internal rotation. If it is touching then vigorous movement can damage femur head so it should not be done in certain cases.
Cast & brace application: Brace or cast application are given in early stage of Perthes to keep femur head inside acetabular cavity. Before application of plaster, we need to assure about position of femoral head inside acetabular cavity. So plaster application is being done in operation theatre and under anaesthesia.
Step of plaster application:
Anaesthesia: short general anaesthesia is required for procedure
Arthrogram: during the procedure series of x-ray will be taken after giving radiopaque dye inside the hip joint by needle. By the arthrogram we will be sure about position of femoral head & congruency
Adductor Tenotomy: in some of the cases, adductor muscle are tight so it will be very difficult to take leg apart for best position of femoral head inside acetabular cavity. In this surgery, doctor will cut tight adductor longus muscle inside of upper thigh by mini incision.
Usually plaster are given for 6- 8 week followed by exercises to increase the range of movement.
Bony surgery:
If weight bearing surface of femoral head is not fully covered by acetabulum then doctor can advise about surgery on femur or acetabulum to cover femoral head
Proximal femur surgery:
Most common procedure is cutting of proximal femur and rotating femoral head in a position that most of the weight bearing position get good coverage by acetabulum. It promote fast healing & give a new chance for rounded head. Bone will be fix with plate & screw.
Acetabular surgery:
Some time it is not possible to cover femoral head by surgery on femur then we need to deepen acetabulum socket by acetabular osteotomy or putting extra bone on side of acetabular margin.
- Medicine is required to treat pain and swelling in the hip joint.
- Rest and exercise are required to improve the movement of the joint.
- Some time plaster and the brace are required to maintain the hip in situ.
- If a child started having pain and slight restriction of hip joint movement then we do a small cut in the adductor area and apply plaster in anesthesia with a leg wide apart.
- With this plaster, the child can have supported walking. This plaster has to be kept for a few months. An abduction brace is useful but very cumbersome for most children. It needed to be wear for months.
Surgical Treatment of Perthes Disease:
The goal of Perthes disease treatment is to reduce painful symptoms, protect the femoral head shape, and restore natural hip movement. In severe cases and children of older age, more than 8 years may need a different kind of pediatric orthopedic surgery.
Surgery is required to place the ball of the femur in the socket of the hip joint.
Type and indication of surgery are based upon a percentage of roundness of femoral head & extrusion of part of the head. In surgery some time need cutting the bone of the femur or pelvis to place the ball in the joint and fixation with a steel plate and screw.
Therapy may be required afterward to improve hip joint movement. There are many Perthes disease treatment options. While developing a treatment plan for your child, your doctor will consider numerous factors.
Prognosis of Perthes Disease:
- Most of the children at a younger age do very well and became nearly normal in due course of time.
- Perthes in older age > 8 years, chances of deformation of the ball is more, that can lead to arthritis in old age.
- Early surgical intervention to contain the hip is very important to maintain sphericity of femoral head.
- If the round surface of the head cannot be maintained by surgery then the outcome will not be good.
For More Information: Pediatric Orthopedic Treatment FAQs


Reference Links :
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4292319/
- https://my.clevelandclinic.org/health/diseases/14587-perthes-disease
- https://en.wikipedia.org/wiki/Legg%E2%80%93Calv%C3%A9%E2%80%93Perthes_disease
- https://orthoinfo.aaos.org/en/diseases–conditions/perthes-disease
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/perthes-disease-leggcalveperthes-disease
Frequently Asked Questions
What are the stages of Perthes disease?
The stages are –
- Initial stage,
- Fragmentation stage,
- Healing period,
- Growing period,
- Definite stage
What happens if Perthes disease is left Un-Treated?
If Perthes Disease is not treated properly, then it can create complications in adulthood, such as early-onset arthritis.
What activities are safe or helpful for my child?
To know better about the activities that are safe and also helpful for your child, you should consult the doctor because it depends on the stage of the disease, symptoms, stiffness of the hip joint, and also the age of the child.
Reviewed and Submitted by Dr. Jitendra Kumar Jain
Last updated on November 27, 2020
Dr.Jitendra Jain, MD and DNB (Orthopedics), president at Trishla Foundation, an NGO for treatment of cerebral palsy, and a Consultant Pediatric Orthopedic Surgeon & Cerebral Palsy Specialist at Trishla Orthopedic Clinic & Rehab Center.
Dr. J. K. Jain is a member of the general council at Dr. SMN university of rehabilitation, Lucknow, a member of the advisory board chief commissioner for PWD, Govt. of India (New Delhi), a member of the state disability research committee (U.P.), and a member of the committee of RCI, New Delhi. He has been awarded many awards, including the Dr.Bhagawan das memorial award, the spirit of humanity award, and the state govt. award for his services towards PWD, etc. Times of India has posted his work many times and mentioned him as one of the best doctors in the field of Pediatric Orthopedics. He helped many children recovering from cerebral palsy, just like comedian jay Chanikara, who is now able to stand and walk without any support, Abena, a Ghana girl with cerebral palsy, and many more. He also organized the National Wheelchair cricket tournament and created World’s first cerebral palsy village foundation in Prayagraj. He successfully treated 10,000+ children with various kinds of orthopedic disability, conducted 160+ free assessment camps, and produced a documentary film on cerebral palsy.
Walk in Appointments Available Daily
You can make an appointment online for video tale-consultation by fixing up an appointment at this website or you can visit the clinic to make an appointment in person and show to doctor with the care of social distancing at the given time.
Contact us
Call Us
0532-2468989
+ 91 9415014994
+ 91 8577873545
+ 91 9455001645
Email Us
totrishlaortho@gmail.com
Our Location
Dr. Jitendra Kumar Jain
Trishla Orthopedic Clinic & Rehab center, 182C / 350A, Tagore Town, Prayagraj (Allahabad) U.P-211002, India
